Scabies Treatment Table of Contents
Understanding Scabies
What Causes Scabies?
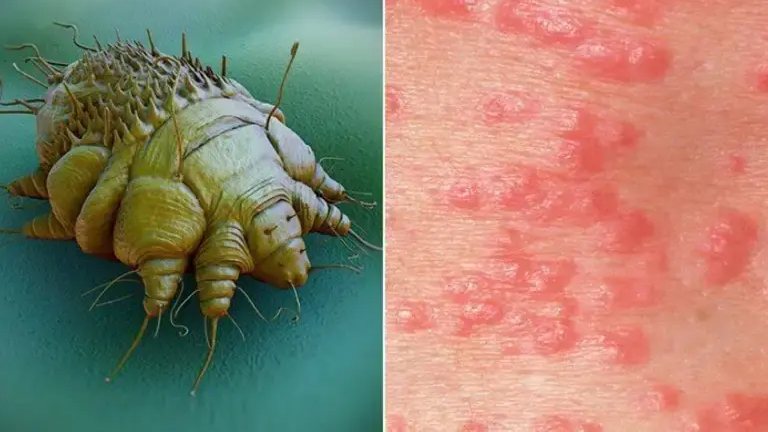
Scabies is caused by an infestation of the Sarcoptes scabiei mite, a tiny, eight-legged parasite invisible to the naked eye. These microscopic mites burrow into the top layer of human skin to lay eggs, causing an immune reaction that leads to intense itching, redness, and rashes. The mites thrive in warm, moist areas of the body, such as between fingers, wrists, elbows, armpits, waistline, and genital regions.
The primary way scabies spreads is through prolonged skin-to-skin contact with an infected person. This means close physical contact in households, schools, childcare centers, and nursing homes can lead to outbreaks. Indirect transmission can also occur through sharing contaminated items like bedding, towels, clothing, and even furniture.
Certain populations are more susceptible, including children, the elderly, and individuals with weakened immune systems. Crowded living conditions and poor hygiene may increase the risk, although scabies can affect anyone regardless of cleanliness.
The incubation period for scabies ranges from 2 to 6 weeks, which means symptoms may not appear immediately after exposure, making early detection and treatment crucial. Understanding the cause is the first step in effective scabies treatment, preventing further spread, and protecting family and community members from infection.
Common Symptoms of Scabies
Recognizing scabies symptoms ensures timely intervention. Typical signs include:
- Itchy rash, often between fingers, wrists, elbows, waist, and underarms
- Small blisters or bumps caused by mite burrowing
- Persistent nighttime itching
- Sores from scratching, leading to bacterial infection if untreated
- Crusted or thickened skin in severe cases (crusted scabies)
How Scabies Spreads
Scabies spreads through direct skin-to-skin contact, or indirectly via contaminated clothing, bedding, or towels. Understanding the scabies contagious period is vital: infected individuals can transmit mites even before symptoms appear.
Medical Treatments for Scabies
Prescription Creams and Ointments
The most effective treatments are prescription scabies cream and ointments:
- Permethrin 5% cream: First-line treatment; apply from neck to toes, leave 8–14 hours, wash off.
- Benzyl benzoate lotion: Alternative for sensitive patients.
- Sulfur ointment: Safe for children and pregnant women.
Consistency is key; repeat applications may be necessary after 7 days.
Oral Medications for Severe Cases
Ivermectin is prescribed for widespread or crusted scabies. Administered orally, it’s repeated after 1–2 weeks. Oral medications are especially useful in outbreaks or when topical treatments fail.
Comparison of Treatments
| Treatment Type | Usage | Pros | Cons |
|---|---|---|---|
| Permethrin Cream | Topical, once or twice | Highly effective, safe for most adults and children | May cause temporary burning or itching |
| Benzyl Benzoate Lotion | Topical, daily for 3 days | Alternative for sensitive skin | Strong odor, skin irritation possible |
| Ivermectin | Oral, 1–2 doses | Effective for severe cases, easy application | Not recommended for pregnant women or children under 15 kg |
| Sulfur Ointment | Topical, daily for 3–5 days | Safe for kids, pregnant women | Messy, strong smell, slower acting |
Home Remedies and Natural Solutions
Tea Tree Oil for Scabies Relief
Tea tree oil is a natural remedy known for its anti-parasitic and anti-inflammatory properties, making it effective in relieving scabies symptoms. It helps kill the mites and soothes the itching and redness caused by the infestation. To use, dilute a few drops of tea tree oil with a carrier oil, such as coconut or olive oil, and apply gently to affected areas once or twice daily. Consistent application can reduce discomfort and support medical treatments. While tea tree oil eases symptoms, it should be combined with prescribed medications for complete scabies eradication.
Neem and Aloe Vera Applications
Neem and aloe vera are natural remedies that help relieve scabies symptoms. Neem has anti-parasitic and antibacterial properties that can reduce mite infestation and prevent infections from scratching. Apply neem paste or neem oil to affected areas daily. Aloe vera gel soothes irritation, reduces redness, and provides a cooling effect. While these remedies help alleviate discomfort, they should be used alongside prescribed medications for complete scabies treatment and prevention of reinfection.
Other Natural Remedies
- Coconut oil to hydrate skin and reduce irritation
- Clove oil for anti-mite effects (diluted with carrier oil)
- Garlic paste applied topically may kill mites naturally
Lifestyle and Hygiene Practices
Complement medical treatments with hygiene practices:
- Wash clothes, bedding, and towels in hot water
- Vacuum mattresses and furniture
- Trim nails to prevent secondary infections
- Shower regularly to remove mites from the skin
Preventing Scabies Reinfection
Cleaning Clothes, Bedding, and Personal Items
Proper cleaning of clothes, bedding, and personal items is essential to prevent scabies reinfection. Wash all fabrics in hot water (at least 50°C) and dry them on a high-heat setting to kill mites and their eggs. Items that cannot be washed, such as stuffed toys or delicate clothing, should be sealed in airtight plastic bags for at least 72 hours, as mites cannot survive without human contact for more than a few days. Regular cleaning and careful handling of personal items complement medical treatments and help ensure that scabies is completely eradicated from the home environment.
Avoiding Close Contact During Infection
Limiting close physical contact is crucial during a scabies infection to prevent spreading the mites to others. Avoid hugging, shaking hands, or sharing beds until treatment is complete. Do not share personal items such as towels, clothing, or bedding, as indirect transmission is common. In households, it is important to temporarily isolate the infected individual while ensuring they receive proper care. Educating family members and roommates about transmission helps reduce the risk of reinfection. Combining contact avoidance with medical treatment and hygiene practices ensures faster recovery and protects others from contracting scabies.
Monitoring Family Members
Monitoring family members is essential to prevent scabies reinfection and household outbreaks. Since scabies spreads easily through prolonged skin-to-skin contact, all close contacts of an infected individual should be observed for symptoms such as itching, rashes, or small bumps. Even if symptoms are mild or not yet present, it’s often recommended that family members undergo preventive treatment simultaneously with the infected person to break the transmission cycle. Regularly inspect clothing, bedding, and personal items for signs of contamination. Educating family members about hygiene practices, avoiding shared items, and early reporting of symptoms helps ensure a safer environment and reduces the risk of recurring scabies infections in the household.
[INSERT_ELEMENTOR id=”5108″]
Scabies in Children and Adults
Differences in Symptoms by Age
Scabies symptoms can vary depending on age, which is important for accurate diagnosis and treatment. In children, rashes often appear on the head, face, scalp, and neck, areas less commonly affected in adults. They may also develop widespread irritation and more pronounced itching due to sensitive skin. In adults, rashes typically appear on the hands, wrists, elbows, waistline, and genital areas. Adults may also experience more localized itching, often worse at night. Understanding these age-related differences ensures that scabies treatment is targeted appropriately, preventing misdiagnosis and allowing for effective relief of itching and infection control.
Safe Treatments for Kids
Treating scabies in children requires special care to ensure safety and effectiveness. The most commonly recommended options are permethrin 5% cream and sulfur ointments, both of which are safe for children, including infants and toddlers. Apply the medication gently to all areas of the body, following the doctor’s instructions, and repeat treatment if necessary. Avoid using harsh chemicals, strong medications, or untested home remedies, as children’s skin is more sensitive and prone to irritation. In addition to topical treatment, maintaining clean clothing, bedding, and hygiene practices helps prevent reinfection. Consulting a pediatrician before starting any treatment ensures safe and proper care for children with scabies.
When to See a Doctor
Signs Your Scabies Infection is Worsening
Seek medical attention if you notice:
- Severe itching that disrupts sleep
- Spreading rash or pustules
- Signs of bacterial infection (pus, fever)
- No improvement after 1–2 weeks of treatment
Complications to Watch Out For
Untreated scabies may lead to:
- Secondary bacterial infections
- Crusted scabies (thick, scaly patches)
- Long-term skin damage
Case Studies and Patient Experiences
Case Study 1: Adult Male with Severe Itching
John, a 34-year-old man living in the USA, developed severe itching and red bumps on his hands, wrists, and waistline after coming into contact with a colleague who had scabies. Initially, he tried home remedies like tea tree oil and neem paste, which provided temporary relief but did not eliminate the mites. After visiting a dermatologist, John was prescribed permethrin 5% cream, applied from the neck down and repeated after one week. He also cleaned his bedding, clothes, and personal items according to recommended hygiene practices. Within two weeks, John experienced significant improvement: the itching reduced, the rash began to heal, and no new bumps appeared. This case highlights the importance of combining medical treatment with hygiene measures for effective scabies eradication, especially in adults with severe symptoms.
Case Study 2: Pediatric Case in Canada
Emma, a 7-year-old girl living in Canada, began showing red, itchy rashes on her scalp, neck, and behind the ears. Her parents initially tried home remedies such as neem paste and aloe vera gel to soothe the itching, but the rash persisted and worsened. After consulting a pediatrician, Emma was diagnosed with scabies. The doctor recommended sulfur ointment, which is safe for children, applied carefully to all affected areas for several consecutive nights.
In addition to topical treatment, her parents followed strict hygiene practices: washing her bedding and clothes in hot water, sealing non-washable items in plastic bags for 72 hours, and preventing close contact with other family members until the treatment was complete. Within ten days, Emma’s itching subsided, and her skin began to heal.
This case emphasizes that early detection, age-appropriate medications, and proper hygiene are crucial in treating scabies in children. Combining safe treatment with preventive measures ensures recovery without reinfection.
Case Study 3: Crusted Scabies in UK Nursing Home
In a nursing home in the UK, several elderly residents developed crusted scabies, a severe and highly contagious form of scabies characterized by thick, scaly skin and intense itching. Due to weakened immune systems and close living conditions, the infestation spread rapidly among residents and staff. The facility immediately contacted healthcare professionals for intervention.
The treatment plan included oral ivermectin combined with topical permethrin 5% cream, applied carefully to all affected residents. Staff were trained in proper application techniques and strict hygiene protocols. Bedding, clothing, and shared items were washed in hot water or sealed in plastic bags for at least 72 hours to eliminate mites from the environment. Residents were temporarily isolated to prevent further transmission.
Within three weeks, the combined treatment successfully eliminated the scabies infestation. The case highlighted the importance of early diagnosis, combined oral and topical treatments, environmental decontamination, and infection control protocols in managing outbreaks in communal settings. This scenario demonstrates that crusted scabies requires intensive and coordinated care to protect vulnerable populations and prevent large-scale outbreaks.
Expert Tips for Fast Recovery
Recovering from scabies quickly requires a combination of medical treatment, hygiene measures, and lifestyle adjustments. Experts recommend applying prescribed topical creams, such as permethrin 5% or sulfur ointment, to all areas of the body, including under nails, skin folds, and between fingers, to ensure no mites survive. Repeat applications as directed by your healthcare provider to target newly hatched mites.
To reduce discomfort, use anti-itch lotions, calamine, or antihistamines to relieve persistent itching and prevent skin damage from scratching. Maintaining clean bedding, clothing, and personal items is crucial; wash fabrics in hot water, dry on high heat, or seal items in plastic bags for 72 hours. Avoid sharing towels, clothes, or bedding to prevent reinfection and transmission.
Experts also advise monitoring household members and treating all contacts simultaneously if needed. Showering before applying medication can improve absorption, and keeping nails trimmed reduces secondary infections from scratching.
By following these expert tips and combining proper treatment with preventive hygiene, scabies can be effectively eliminated, itching relieved, and the risk of reinfection minimized. Early intervention and diligence are key to fast recovery.
Country-Specific Guidelines
Scabies treatment guidelines vary slightly by country, reflecting local healthcare recommendations and available medications. Understanding these guidelines ensures safe and effective care.
USA:
The Centers for Disease Control and Prevention (CDC) recommends permethrin 5% cream as the first-line treatment for scabies. In cases of widespread or crusted scabies, oral ivermectin may be prescribed. Household contacts should be treated simultaneously to prevent reinfection. Emphasis is placed on thorough cleaning of bedding, clothing, and personal items to reduce transmission.
UK:
The National Health Service (NHS) advises using permethrin cream or malathion lotion for scabies treatment. Crusted scabies requires a combination of oral ivermectin and topical creams. Care homes and communal facilities follow strict infection control measures, including temporary isolation of affected residents and environmental decontamination.
Canada:
Health Canada recommends permethrin 5% cream as the standard treatment, with oral ivermectin for severe or resistant cases. Pediatric and elderly patients require special consideration for dosage and safety. All close contacts should be monitored and treated if necessary.
Across all countries, the core principles remain consistent: early diagnosis, proper application of treatment, environmental cleaning, and monitoring household or community contacts. Following country-specific recommendations ensures that scabies is effectively eliminated, reduces the risk of outbreaks, and provides guidance tailored to local healthcare standards.
[INSERT_ELEMENTOR id=”5745″]
Common Myths vs Facts About Scabies
Myth 1: Scabies Only Affects Dirty People
Fact: Scabies can affect anyone, regardless of hygiene. The mites spread through contact, not cleanliness.
Myth 2: Scabies Can Go Away Without Treatment
Fact: Without treatment, scabies persists and worsens. Medical intervention is essential.
Myth 3: Home Remedies Alone Can Cure Scabies
Fact: Natural remedies may relieve itching, but complete eradication requires medical treatments.
FAQs About Scabies Treatment
1. How Long Does Scabies Itching Last After Treatment?
Even after the mites are killed, itching can persist for 2–4 weeks due to an allergic reaction to dead mites. Anti-itch creams or antihistamines can help relieve discomfort during this period.
2. Can Scabies Go Away Without Treatment?
No. Without proper treatment, scabies persists and worsens, causing intense itching and increasing the risk of secondary bacterial infections. Medical intervention is necessary for complete eradication.
3. Are Permethrin Creams Safe for Children and Pregnant Women?
Yes, permethrin 5% cream is generally safe for both children and pregnant women. Always follow a doctor’s instructions for proper application and dosage.
4. Can Home Remedies Alone Cure Scabies?
Home remedies, such as tea tree oil or neem paste, soothe symptoms but cannot completely eliminate the mites. They should be used as supportive care alongside prescription treatments.
5. How Is Scabies Spread?
Scabies spreads through prolonged skin-to-skin contact or sharing contaminated items like clothing, bedding, or towels. Early detection and treatment help prevent outbreaks.
6. What Is Crusted Scabies?
Crusted scabies is a severe form characterized by thick, scaly patches and high mite counts. It requires combined oral and topical treatments and strict hygiene measures to prevent rapid transmission.
7. How Can I Prevent Reinfection?
Wash all clothing, bedding, and personal items in hot water, disinfect your living environment, avoid close contact during treatment, and monitor household members. Treating all contacts simultaneously is recommended to prevent reinfection.