🕥 Estimated reading time: 16 minutes
Get the real story on measles outbreak causes and prevention—why they happen, how the virus actually spreads, and what puts people most at risk. Learn to spot the symptoms, understand the complications, and see why vaccination matters. Hear what the experts are saying, look at what’s going on around the world, and find out what public health teams are doing to keep both kids and adults safe. Staying up to date helps you protect your community—and yourself—from measles.
Clickable Chapter Summaries
Acquaintance to Measles and Why Outbreaks Matter
Measles spreads fast—almost too fast. The Measles morbillivirus causes it, and honestly, public health experts still wrestle with it everywhere. We’ve got vaccines that work and aren’t hard to get, but somehow, outbreaks keep showing up—in the U.S., the U.K., Canada, and in countries with less access to healthcare. If we want to stop measles from getting out of hand, people need to understand what sparks these outbreaks and what actually shuts them down. When folks know what’s going on, everyone—from individuals to whole communities—can pitch in and help keep this disease under control.
The Global Burden of Measles
Measles Outbreak Causes and Prevention: Measles still takes the lives of far too many young children around the world, especially in places where not enough kids get vaccinated. According to the World Health Organisation, millions of children face the risk every year, and thousands die from complications like pneumonia, brain swelling, or even severe malnutrition. Lately, measles cases have been climbing again, which really shows how much vaccine hesitancy, migration, and unequal access to healthcare keep getting in the way.
Why Understanding Outbreaks is Crucial
Measles outbreaks aren’t just about people getting sick. They jam up hospitals, put off regular appointments, and sometimes even close schools. Suddenly, everything feels upside down. Things don’t just sort themselves out, either—you need fast action and solid prevention to keep things from getting worse. That’s exactly why public health experts spend so much time figuring out how these outbreaks begin and, even more importantly, how to shut them down.
How Measles Starts and Spreads
Measles spreads mostly when someone with the virus coughs, sneezes, or just talks, sending tiny droplets into the air. Those germs can hang around—on surfaces or floating in the air—for up to two hours. That’s part of what makes measles so contagious. Knowing how it spreads isn’t just good for protecting yourself; it’s a big deal for public health, too.
Airborne and Droplet Transmission
Measles moves fast, mostly through tiny droplets in the air. When someone with measles coughs or sneezes, people nearby can easily breathe in the virus. Packed places like classrooms, hospitals, or buses? The virus loves those. It spreads like wildfire there. Research puts measles’ basic reproduction number, or R0, somewhere between 12 and 18. So, one sick person can pass it on to a dozen people, sometimes more. That’s why getting enough people vaccinated really matters. Herd immunity isn’t just a nice idea — it’s what keeps outbreaks from spiraling out of control.
Direct Contact and Surface Contamination
Measles usually spreads through the air, but it can also pass from person to person by touching stuff like doorknobs or utensils that have an infected person’s nasal or throat secretions on them. The virus sticks around on these surfaces for a bit, which makes it easier for measles to move quickly through groups of people. That’s why good hygiene matters just as much as getting vaccinated.
The Role of Immunity Gaps
Outbreaks usually happen when there are holes in a community’s immunity. Sometimes it’s because not everyone gets vaccinated. Other times, people’s immunity just fades over time. Kids who are too young for the vaccine and anyone unvaccinated face the biggest risks. When public health teams know exactly where these gaps are, they can focus their vaccination efforts and stop outbreaks before they get out of hand.
Population Dynamics and Mobility
People moving around—migrating, travelling, even being displaced—drive the spread of measles more than you might think. When someone brings measles into a place that hasn’t seen it in years, one case can spark a whole outbreak. That’s why countries need to work together and set vaccination rules for anyone crossing borders. Packed cities and crowded spaces just make things worse, letting the virus jump from person to person in no time.
Seasonality and Environmental Factors
Seasonal and environmental factors play a big role in how measles spreads. In places with temperate climates, you see more outbreaks in winter and early spring. People stay inside more, windows stay shut, and the air doesn’t move much—so the virus finds it easier to jump from person to person. In tropical areas, outbreaks often line up with the rainy season. It’s a good example of how the weather and the way people live combine to shape how measles moves through a community.
Preventing Spread Through Awareness and Behaviour
Knowing how measles spreads helps people and communities protect themselves. When someone shows symptoms, it’s important to keep them isolated right away. Staying away from crowds during an outbreak and keeping up with good hygiene also help, along with getting vaccinated. Public health campaigns really make a difference by getting the word out about what people can do.
In Section 1, we looked at why measles outbreaks happen and how to prevent them. We talked about how common measles is around the world, how it spreads, and where immunity gaps exist. Population movement and the environment matter, too. All of this sets us up to dive deeper into the main risk factors and what’s happening with measles globally.
Key Risk Factors Behind Measles Outbreaks
If we want to stop measles outbreaks, we have to figure out what’s actually causing them. Measles spreads fast, but these outbreaks don’t just pop up out of nowhere. Things like people’s immunity, how communities interact, and even the environment all play a part. When health officials and communities spot these risk factors early, they can take steps to keep outbreaks from hitting so hard—anywhere in the world.
Low Vaccination Coverage
Not getting enough people vaccinated is a huge problem. To stop measles from spreading, about 95% of everyone needs their shots. If a community falls short of that, it’s wide open for an outbreak. The World Health Organisation points to low vaccination rates as the main reason measles is coming back, not just in poorer countries, but also in places like the US, UK, and Canada.
Vaccine Hesitancy and Misinformation
In a lot of wealthy countries, misinformation has made people more hesitant about vaccines, and that’s led to outbreaks popping up locally. When people don’t trust vaccines or believe the wrong things about their safety—or when certain cultural beliefs come into play—you end up with groups who don’t get vaccinated at all. Those clusters become perfect spots for diseases to spread. The best way to fight this is with public health campaigns that focus on real education, building trust, and sharing reliable information.
Population Density and Urban Crowding
When a lot of people live close together, measles spreads fast. Cities packed with crowded schools, busy buses and trains, and bustling markets pretty much give the virus everything it wants. In places like that, researchers have watched measles sweep through and infect nearly every person who isn’t immune—sometimes in just a few weeks.
Migration, Displacement, and Refugee Populations
When conflict, disasters, or economic struggles force people to move, outbreaks become a real risk. Refugee camps and makeshift shelters usually deal with cramped spaces, bad sanitation, and not enough vaccines to go around. UNICEF points out that running immunisation campaigns focused on these displaced communities stops outbreaks before they spiral out of control.
Malnutrition and Vitamin A Deficiency
Kids who don’t get enough nutrition—especially vitamin A—tend to get hit harder by measles. They’re more likely to end up with serious problems like pneumonia or encephalitis. That’s why public health teams usually pair vitamin A supplements with measles vaccines. It’s a smart move that saves lives, especially in countries where resources are tight.
Weak Healthcare Infrastructure and Surveillance Gaps
Weak healthcare systems and poor surveillance let outbreaks slip through the cracks. Catching problems early, reporting them fast, and jumping into action are key to stopping things from getting out of hand. You can see the difference—countries that keep a close eye on potential threats usually keep outbreaks from spiraling. That’s why steady investment in public health and solid monitoring matters so much.
Recent Global Trends in Measles Outbreaks
We’ve made a lot of progress fighting measles, but outbreaks still pop up all over the world—even in countries with plenty of resources. This isn’t just a local problem; it’s global. If we want to get ahead of it, we need to work together and come up with prevention strategies that actually stick.
High-Income Countries
Even in places like the US, UK, and Canada—where most people get vaccinated—outbreaks still pop up. Usually, it’s because small groups of people skip their shots, often because they’re hesitant about vaccines. These gaps in local immunity can mess with the bigger picture, even if the country as a whole looks well protected. Focusing on targeted vaccination drives and school-based programs really helps stop these outbreaks before they spread.
Low- and Middle-Income Countries
Measles spreads more easily in low- and middle-income countries. People there often struggle to get healthcare, and getting vaccines out to everyone isn’t simple. Other health problems sometimes take priority, too. WHO and UNICEF have stepped in with big vaccination drives that really help keep outbreaks in check. Still, some places—especially where there’s conflict—keep slipping through the cracks.
Impact of Global Travel and Connectivity
When people travel around the world, they can bring measles into places that haven’t seen it in years. All it takes is one person who’s infected—if enough people nearby aren’t protected, measles spreads fast. That’s why countries rely on vaccination rules and try to keep travellers informed. These steps help stop measles from jumping borders and causing new outbreaks.
Seasonal and Environmental Factors
Measles spreads differently depending on the season. In places with temperate climates, outbreaks pop up more often in winter, mostly because people spend more time indoors together. In tropical areas, it’s the rainy season that ramps things up—everyone crowds inside, and the environment just makes it easier for the virus to get around.
Public Health Policy and Global Initiatives
Thanks to global efforts like the Measles & Rubella Initiative, far fewer people die from measles now. Countries that stick to solid vaccination schedules, keep a close eye on disease trends, and act fast when outbreaks pop up—these places just don’t see as many big, out-of-control outbreaks. Keeping up the momentum means we still need to invest in public health systems and keep those vaccination programs running strong.
Case Studies Highlighting Global Trends
Look at what’s happened lately—in Ukraine back in 2019, plus plenty of places across North America and Africa. These outbreaks really show what happens when vaccination rates drop, or when public health systems can’t keep up, or when social issues get in the way. Every outbreak underlines how much targeted action, quick responses, and real teamwork across countries matter if we want to stop things from getting worse next time.
In Section 2, the report took a hard look at the main reasons measles still breaks out: missing vaccinations, crowded cities, people on the move, malnutrition, and weak disease tracking. It also covered bigger global patterns, pointing out that measles is making a comeback in rich and poor countries alike. Bottom line: we need to work together, with smart public health plans, if we want to keep measles in check.
Symptoms, Complications, Prevention & Vaccination Strategies
Measles Outbreak Causes and Prevention: Measles hits hard—it’s a viral illness that comes with obvious symptoms and some real risks if things go wrong. Knowing what to look for and how to protect yourself really matters, especially if we want to keep outbreaks in check around the world. The best way to stop measles? Combine solid public health info, personal safety steps, and strong community vaccination efforts. That’s what keeps this disease from spreading.
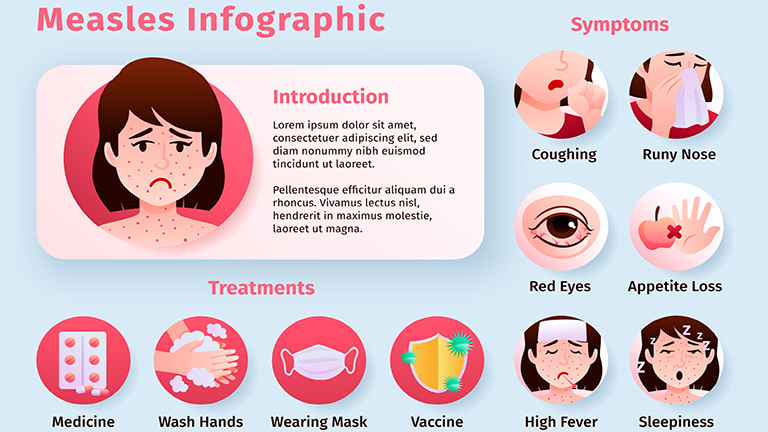
Recognising Measles Symptoms
Measles usually takes about 10 to 14 days to show up after you’re exposed. At first, it feels a lot like any mild virus—fever, a cough, runny nose, maybe those red, watery eyes. Then, a few days in, that classic red, blotchy rash shows up. It starts on your face and then spreads down to your body and arms and legs. Catching these signs early really matters—you want to act fast to keep it from spreading.
Common Complications of Measles
Measles usually runs its course, but it can get pretty serious, especially for kids under five or anyone with a weak immune system. Some of the most common problems? Pneumonia, brain swelling (that’s encephalitis), ear infections, bad diarrhea, and sometimes really dangerous dehydration.
Prevention of Measles Outbreaks
How do you stop measles from spreading? It mostly comes down to making sure people get vaccinated, keeping everyone informed, and jumping in fast with public health actions when cases pop up. These steps are key if we want to keep measles under control around the world.
Vaccination: The Cornerstone of Prevention
The measles vaccine—usually given as part of the MMR shot—does the best job at stopping outbreaks. You need two doses for solid, long-term protection. When enough people get vaccinated, especially if coverage hits 95% or more, the whole community stays safer because the disease can’t spread easily. It’s not just about protecting yourself; you’re actually helping everyone around you.
Mass Immunisation Campaigns
When coverage drops or outbreaks hit, health teams roll out mass vaccination campaigns. They focus on kids and people most at risk, trying to close those immunity gaps fast. WHO and UNICEF have pulled off some huge campaigns across Africa, Asia, and parts of Europe—and you can see the results in lower case numbers and fewer deaths.
Post-Exposure Prophylaxis
If someone’s exposed to measles, acting fast makes a difference. Get them vaccinated within 72 hours or give immunoglobulin—it can stop the disease or at least make it less severe. Quick action really matters during outbreaks, especially in places like schools, hospitals, or crowded neighbourhoods.
Community and Public Health Measures
Vaccination is the main defence, but it’s not the only one. Public health teams also work to keep the virus from spreading. They isolate people who are sick, trace who they’ve been in contact with, and push for better ventilation in schools and hospitals. They run education campaigns so people know why immunisation matters and how to spot symptoms early. When communication is clear, communities are more likely to take these steps seriously.
Tackling Vaccine Hesitancy
Getting people on board with vaccines takes more than just facts—it’s about connecting with communities, building trust with doctors and nurses, and making sure reliable info reaches everyone. In places where rumors and misinformation spread fast, especially in wealthier countries, this kind of outreach really matters. If people trust their healthcare providers and understand the science, they’re much more likely to get vaccinated.
Nutrition and Supportive Care
Good nutrition goes hand in hand with fighting illnesses like measles. Kids need enough vitamins, especially vitamin A, to help their immune systems stay strong and bounce back faster if they do get sick. That’s why public health teams often pair nutrition programs with vaccination clinics, especially in areas where kids are at higher risk.
Global Vaccination Strategies
Every country has its own playbook for keeping vaccination rates up. Some make sure shots are part of the school routine, others run special catch-up drives or tie vaccines into regular doctor visits. The CDC says sticking to the recommended vaccine schedule is key, and they urge travellers to get their shots so they don’t bring measles back home.
Case Studies of Successful Prevention
The Americas managed to eliminate measles for a while, and they did it with widespread vaccination and serious tracking of every case. Their approach—big-picture planning, getting communities involved, and working together across borders—shows what it takes to keep measles away.
Section 3 covered what measles looks like, the problems it can cause, and all the ways to prevent it—from vaccines and quick action after exposure, to community programs and nutrition support. Pulling all these pieces together is how we keep measles outbreaks under control everywhere.
Expert Opinions on Measles Outbreak Causes and Prevention
Measles Outbreak Causes and Prevention: Global experts emphasise that measles outbreaks are preventable but require sustained public health investment, education, and high vaccination coverage. Dr. Tedros Adhanom Ghebreyesus, Director-General of the World Health Organisation (WHO), notes that “measles deaths are a tragedy in the 21st century, as safe and effective vaccines are widely available. Every child should be vaccinated to prevent these unnecessary deaths.”
Insights from CDC Experts
The Centers for Disease Control and Prevention (CDC) underscores that measles outbreaks in the US are largely driven by clusters of unvaccinated individuals. CDC experts recommend routine two-dose MMR vaccination for all children and adults without evidence of immunity, rapid response to imported cases, and strong public education campaigns to counter misinformation.
UNICEF Recommendations
Measles Outbreak Causes and Prevention: UNICEF highlights the vulnerability of children in displaced populations and emphasises integrated immunisation and nutritional programs. Experts recommend mass vaccination campaigns combined with vitamin A supplementation and community engagement to prevent severe measles complications.
Global Health Research Insights
Measles Outbreak Causes and Prevention: Peer-reviewed studies confirm that outbreaks are most severe in areas with low immunisation coverage, population displacement, or weak healthcare infrastructure. For example, research published on PubMed shows that measles transmission in urban slums and refugee camps is facilitated by overcrowding, poor sanitation, and malnutrition, highlighting the need for targeted interventions.
Conclusion Measles Outbreak Causes and Prevention
Measles is still a real threat around the world, even though we have vaccines that work. Outbreaks happen for all sorts of reasons—some people don’t get vaccinated, others are hesitant, and then there’s overcrowding, people moving from place to place, and poor nutrition. Stopping measles takes more than just shots. It’s about getting vaccines out there, teaching communities, keeping an eye on new cases, acting fast when outbreaks start, and making sure people get the nutrition they need. Countries that do the best job are the ones that keep vaccination rates high, invest in solid healthcare, and earn people’s trust.
If we want to beat measles globally, we have to keep funding public health, stick to proven ways of getting people vaccinated, and make sure everyone can actually get the vaccine. Protecting yourself matters, but so does working together and following the recommended vaccination schedule. That’s how we keep outbreaks from coming back and protect the people who need it most.
FAQ Measles Outbreak Causes and Prevention