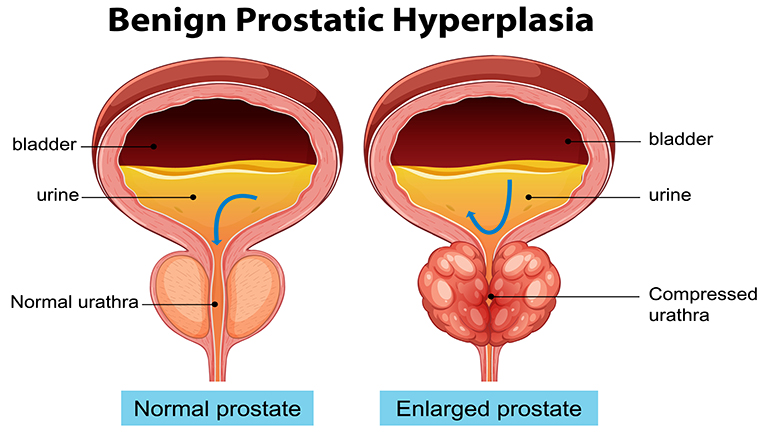
Benign Prostatic Hyperplasia, commonly referred to as BPH, is a medical condition in which the prostate gland, located just below the bladder in men, begins to enlarge. Unlike prostate cancer, BPH is non-cancerous, but the growth of the prostate can cause significant urinary and reproductive issues. The prostate plays a crucial role in producing seminal fluid, and when it enlarges, it can put pressure on the urethra, resulting in difficulty urinating and other urinary symptoms.
The condition is primarily age-related, typically affecting men over the age of 50, but younger men can also develop BPH in rare cases. Understanding BPH is essential because it directly impacts quality of life, affecting sleep, daily routines, and overall health.
How Common is Benign Prostatic Hyperplasia?
Benign Prostatic Hyperplasia is one of the most common urological conditions in aging men. Statistics indicate that nearly 50% of men in their 50s show signs of prostate enlargement, and this prevalence increases to nearly 90% by the age of 80. The condition often develops gradually, and many men may not notice symptoms in the early stages. However, the risk of developing complications such as urinary retention, kidney problems, and recurrent urinary tract infections increases as the condition progresses.
Risk Factors and Causes
Several factors contribute to the development of BPH. Age remains the most significant risk factor, as hormonal changes over time, particularly in testosterone and dihydrotestosterone (DHT) levels, affect prostate growth. Family history also plays a role; men with relatives who have had BPH are at higher risk. Other contributing factors include obesity, diabetes, heart disease, and lifestyle factors such as diet and lack of physical activity.
Hormonal imbalances, specifically an increase in DHT, a metabolite of testosterone, promote prostate cell growth and can trigger BPH development. Understanding these factors helps men take preventive measures and seek timely medical intervention to manage symptoms effectively.
Recognising Symptoms of BPH
Early Signs of an Enlarged Prostate
The early signs of BPH may be subtle but progressively interfere with normal urinary function. Men may notice a weak urine stream, the need to strain while urinating, or a feeling of incomplete bladder emptying. Nighttime urination, known as nocturia, is another common early indicator, often disrupting sleep and reducing overall quality of life.
Additionally, urinary urgency, or a sudden need to urinate, may become more frequent. Men experiencing these early signs should consult a healthcare professional, as early detection can prevent complications and improve long-term outcomes.
Urinary Symptoms and Complications
As BPH progresses, urinary symptoms become more pronounced. Difficulty starting urination, dribbling at the end of urination, and frequent trips to the bathroom may interfere with daily activities. Some men may experience urinary retention, where the bladder cannot empty completely, leading to discomfort and increased risk of urinary tract infections.
Complications of untreated BPH include bladder stones, recurrent urinary tract infections, and in severe cases, kidney damage due to prolonged obstruction. Men experiencing severe urinary symptoms should seek medical attention promptly to prevent irreversible complications.
When to See a Doctor
Men should consult a doctor if they experience persistent urinary symptoms, blood in the urine, or pain during urination. Early medical intervention allows for accurate diagnosis, appropriate treatment planning, and monitoring of potential complications. Regular checkups are recommended for men over 50, even if symptoms are mild, as early detection of BPH significantly improves treatment outcomes.
Diagnosis of Benign Prostatic Hyperplasia
Physical Examination and Medical History
The first step in diagnosing BPH typically involves a thorough medical history and physical examination. A healthcare provider will assess urinary symptoms, review personal and family medical history, and perform a digital rectal exam (DRE) to evaluate the size and condition of the prostate.
During a DRE, the physician palpates the prostate through the rectal wall to identify enlargement or irregularities. While a DRE cannot confirm BPH alone, it provides valuable information to guide further diagnostic tests.
Lab Tests and Imaging
Laboratory tests play an essential role in BPH diagnosis. Urinalysis helps detect urinary tract infections, blood in the urine, or other abnormalities. Blood tests, such as measuring prostate-specific antigen (PSA), are also performed to rule out prostate cancer, as elevated PSA levels can indicate either BPH or malignancy.
Imaging studies like ultrasound or MRI may be used to assess prostate size, bladder function, and identify any complications such as kidney damage. These tests provide a comprehensive understanding of the condition and help tailor treatment plans.
Urodynamic Tests
Urodynamic tests are specialised assessments that evaluate how well the bladder and urethra store and release urine, providing critical insights for men with Benign Prostatic Hyperplasia (BPH). These tests measure urine flow rate, bladder pressure, and the efficiency of bladder emptying. They are especially useful when symptoms are severe, atypical, or do not respond to initial treatments.
Common urodynamic procedures include uroflowmetry, which measures the speed and volume of urination, and cystometry, which assesses bladder capacity and pressure during filling. By identifying functional issues, urodynamic tests help physicians distinguish BPH from other urinary disorders, guide personalised treatment plans, and predict the effectiveness of medications, minimally invasive therapies, or surgical interventions. Accurate testing ensures better long-term management and improved quality of life.
Treatment Options for BPH
Lifestyle Modifications and Home Remedies
Lifestyle changes can significantly improve BPH symptoms and reduce disease progression. Dietary adjustments, such as reducing caffeine and alcohol intake, can decrease urinary frequency. Staying hydrated is essential, but fluid intake should be managed in the evening to reduce nighttime urination.
Regular physical activity strengthens bladder function and promotes overall prostate health. Weight management also helps, as obesity is linked to worsened BPH symptoms. In some cases, herbal supplements such as saw palmetto, beta-sitosterol, or pygeum may offer symptom relief, though clinical evidence varies.
Medications for BPH Management
Medications are commonly used to manage BPH, with two primary classes: alpha-blockers and 5-alpha-reductase inhibitors. Alpha-blockers, such as tamsulosin, relax the muscles around the prostate and bladder neck, improving urine flow.
5-alpha-reductase inhibitors, like finasteride, work by shrinking the prostate over time, reducing obstruction. Combination therapy may be recommended for men with moderate to severe symptoms. It is essential to consult a physician for the appropriate medication and dosage, considering potential side effects such as dizziness, sexual dysfunction, or lowered blood pressure.
Minimally Invasive Procedures
For men whose symptoms do not respond to medication, minimally invasive procedures may be considered. Transurethral microwave therapy (TUMT), transurethral needle ablation (TUNA), and water vapor therapy use heat or energy to reduce prostate tissue and improve urinary flow.
These procedures generally have shorter recovery times compared to traditional surgery and are performed on an outpatient basis. Men considering these treatments should discuss potential risks, effectiveness, and suitability with their urologist.
Surgical Options for Severe Cases
In severe cases of BPH, surgery may be necessary to remove or reduce prostate tissue. Transurethral resection of the prostate (TURP) is the gold standard, involving the removal of part of the enlarged prostate to relieve obstruction.
Other surgical options include laser therapy, open prostatectomy, and robotic-assisted procedures. Surgery is typically recommended for men with significant urinary retention, recurrent infections, or kidney damage. Postoperative care and monitoring are crucial to ensure long-term symptom relief and prevent complications.
Prevention and Long-Term Management
Diet and Exercise for Prostate Health
Maintaining a healthy diet rich in fruits, vegetables, and whole grains supports prostate health. Foods high in antioxidants, such as tomatoes, berries, and green leafy vegetables, can reduce inflammation and promote overall well-being.
Regular exercise improves cardiovascular health, reduces obesity, and supports hormonal balance, all of which contribute to lowering the risk of BPH progression. Men are encouraged to engage in moderate physical activity, such as walking, swimming, or resistance training, for at least 150 minutes per week.
Regular Checkups and Monitoring
Men over 50 or those with risk factors for BPH should schedule regular checkups with a urologist. Monitoring prostate size, urinary symptoms, and PSA levels allows for early detection of progression or complications. Early intervention often leads to better outcomes and can prevent the need for invasive treatments.
Managing Symptoms Naturally
Natural symptom management may include pelvic floor exercises, bladder training, and herbal supplements. Men should discuss these approaches with a healthcare provider to ensure safety and effectiveness. Techniques such as double voiding, where the bladder is emptied twice in succession, can reduce urinary retention and improve comfort.
Complications and Risks
Urinary Retention and Kidney Issues
Chronic urinary retention is a serious complication of Benign Prostatic Hyperplasia (BPH), occurring when the enlarged prostate obstructs urine flow, preventing the bladder from emptying completely. Over time, this can lead to bladder distention, increased risk of urinary tract infections, and the formation of bladder stones. If left untreated, persistent obstruction may cause back pressure on the kidneys, resulting in hydronephrosis or kidney damage. Early detection and management of urinary retention are crucial to prevent long-term renal complications. Treatments may include medications to relax the prostate, minimally invasive procedures, or surgical interventions to restore normal urine flow and protect kidney health.
Impact on Quality of Life
Benign Prostatic Hyperplasia (BPH) can significantly affect a man’s quality of life. Frequent urination, especially at night, disrupts sleep, leading to fatigue, irritability, and reduced productivity. Urinary urgency and incontinence may cause embarrassment, anxiety, and social withdrawal, impacting personal and professional life. Sexual dysfunction, sometimes associated with BPH or its treatments, can further affect emotional well-being and intimate relationships. The persistent discomfort and inconvenience of symptoms may also contribute to stress and mental health challenges. Effective management through lifestyle changes, medications, or surgical interventions can improve urinary function, restore normal routines, and enhance overall quality of life for men with BPH.
BPH vs Prostate Cancer: Key Differences
While BPH and prostate cancer share some symptoms, such as urinary obstruction, they are distinct conditions. BPH is non-cancerous and usually grows slowly, while prostate cancer can be aggressive and requires different management strategies. PSA testing, imaging, and biopsies help differentiate between the two, emphasising the importance of accurate diagnosis.
Expert Tips and Recommendations
Managing Benign Prostatic Hyperplasia (BPH) effectively requires a combination of medical guidance, lifestyle adjustments, and proactive monitoring. Experts recommend that men experiencing urinary symptoms consult a urologist promptly to determine the severity of prostate enlargement and explore treatment options tailored to individual needs. Early intervention often prevents complications such as urinary retention, infections, and kidney damage.
Lifestyle changes play a critical role in symptom management. Regular exercise, maintaining a healthy weight, limiting caffeine and alcohol intake, and practising bladder training can significantly improve urinary function. Men are also advised to stay hydrated but avoid excessive fluid intake before bedtime to reduce nighttime urination.
For those considering medications or minimally invasive procedures, it’s essential to discuss potential side effects, effectiveness, and long-term outcomes with a healthcare provider. Regular follow-ups, PSA monitoring, and adherence to prescribed treatments ensure optimal management, improved quality of life, and long-term prostate health.
Conclusion: Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia (BPH) is a common and manageable condition affecting millions of men worldwide. Early recognition of symptoms, such as urinary frequency, weak urine flow, or nighttime urination, is crucial for preventing complications and maintaining overall prostate health. Timely medical evaluation allows men to choose from a variety of treatment options, including lifestyle changes, medications, minimally invasive procedures, and surgery, tailored to individual needs and symptom severity.
In addition to medical interventions, maintaining a healthy lifestyle plays a pivotal role in managing BPH. Regular exercise, a balanced diet rich in fruits and vegetables, staying hydrated, and avoiding excessive alcohol or caffeine can significantly improve urinary function and quality of life. Men are encouraged to schedule regular checkups with a urologist to monitor prostate health and prevent progression.
For further information and expert guidance on managing BPH, you can explore the following trusted resources:
-
Mayo Clinic: Benign Prostatic Hyperplasia (BPH) – Comprehensive overview of symptoms, causes, and treatment options.
-
Cleveland Clinic: Enlarged Prostate (BPH) – Expert insights on diagnosis, medications, and surgical solutions.
-
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Research-backed resources on long-term management and prevention strategies.
Understanding BPH and taking proactive steps ensures men can lead active, healthy lives while minimizing urinary complications. Early intervention, guided by professional medical advice, is the key to effective management and long-term prostate health.